Disclaimer: This post is for academic purposes only. Please read the original document if you intend to use them for clinical purposes.
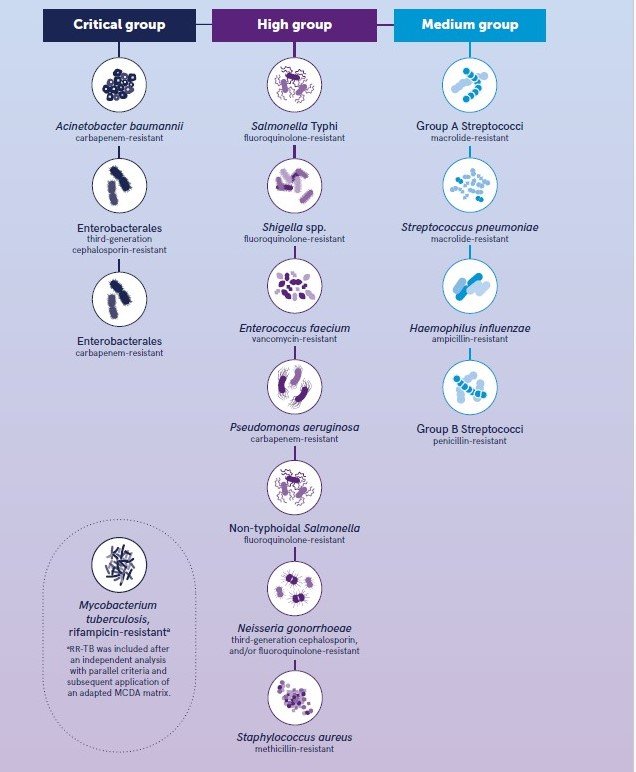
This document summarizes the key themes and important information presented in the World Health Organization’s (WHO) BPPL for 2024. This updated list identifies antibiotic-resistant (ABR) bacterial pathogens of significant public health importance to guide research & development (R&D), and strategies to prevent and control antimicrobial resistance (AMR). It categorizes 15 families of ABR pathogens into critical, high, and medium priority levels. A notable inclusion in the critical priority category is rifampicin-resistant Mycobacterium tuberculosis (RR-TB), which was assessed through a tailored independent analysis and subsequently using a modified Multi-Criteria Decision Analysis (MCDA) approach. The list also reflects an increased recognition of “community” pathogens with rising resistance and global burden, particularly in low- and middle-income countries (LMIC). The document details the methodology used for prioritization, including a global survey to determine criteria weights, and emphasizes the importance of considering regional and local contexts for effective implementation of the BPPL.
Main themes and important facts
-Updated BPPL:
It includes 15 families of antibiotic-resistant pathogens, categorized into critical, high, and medium priority for R&D and public health measures.
- Critical Priority: This category includes Gram-negative bacteria resistant to last-resort antibiotics e.g., carbapenem-resistant Acinetobacter baumannii (CRAB) and carbapenem-resistant Enterobacterales (CRE), as well as third-generation cephalosporin-resistant Enterobacterales (3GCRE) and rifampicin-resistant (RR) Mycobacterium tuberculosis. These pathogens are prioritized due to their ability to transfer resistance genes, the severity of the infections they cause, and their significant global burden, especially in LMIC.
- High Priority: This category includes Enterobacterales (carbapenem-resistant), Salmonella Typhi (fluoroquinolone-resistant), Shigella spp. (fluoroquinolone-resistant), Non-typhoidal Salmonella (fluoroquinolone-resistant), Neisseria gonorrhoeae (MDR, including fluoroquinolone and third-generation cephalosporin resistance), and Enterococcus faecium (vancomycin-resistant). The inclusion of Salmonella and Shigella as high priority reflects their increasing resistance and high infection burden, particularly in LMIC.
- Medium Priority: This category includes Haemophilus influenzae (Ampicillin-resistant), Streptococcus pneumoniae (Macrolide-resistant), Staphylococcus aureus (Methicillin-resistant, i.e. MRSA), Group B Streptococci (Penicillin-resistant), and Mycobacterium tuberculosis (Rifampicin-resistant).
- Note: RR-TB is listed in both critical and medium groups due to the independent assessment and subsequent Multi-Criteria Decision Analysis (MCDA).
-Rationale and Background:
- Antimicrobial resistance is a major threat to public health, modern medicine, and the achievement of Sustainable Development Goals.
- In 2019, an estimated 1.27 million deaths were directly attributable to antibiotic-resistant bacteria, with an additional 5 million associated deaths.
- The first BPPL was developed in 2017 to guide investment in R&D of new antibacterials. The 2024 update builds upon this. The BPPL has been instrumental in guiding R&D investments, leading to the market introduction of nine new antibiotics effective against “critical” priority pathogens from the 2017 list.
- A new anti-TB drug, Pretomanid, has also been introduced and recommended by WHO for MDR-TB and RR-TB treatment.
-Methodology for Prioritization:
A Multi-Criteria Decision Analysis (MCDA) approach was used to prioritize pathogens. This involved:
- Refinement and definition of assessment criteria.
- Identification of experts (WHO BPPL Advisory Group).
- Review of available evidence to establish criteria levels and describe pathogens.
- Conducting a global PAPRIKA (Potentially All Pairwise Rankings of all possible Alternatives) survey to determine the weight of each criterion. 79 experts from all six WHO regions participated.
- Assessment of pathogens against the defined criteria.
- Final scoring, ranking, and evaluation, including sensitivity analysis.
- Eight criteria were used for assessment (weights from the PAPRIKA survey are provided in bracket):
- Mortality (15%)
- Treatability (20%) – Highest weight.
- Trend of resistance (12%)
- Preventability (12%)
- Incidence (11%)
- Transmissibility (11%)
- Non-fatal health burden (11%)
- Pipeline (8%) – Lowest weight.
- RR-TB was initially assessed independently using tailored criteria due to the unique characteristics of TB (chronic course, transmission dynamics, treatment with four or more drugs for at least 6 months). Later, the MCDA method used for other pathogens was also applied to RR-TB, although this post-hoc analysis had some limitations and did not receive unanimous support for all criteria assignments. The final grouping of RR-TB reflects both assessment approaches.
-Key Outcomes and Specific Pathogen Highlights:
- Gram-negative bacterial pathogens resistant to last-resort antibiotics remain a critical priority.
- RR-TB is a critical AMR pathogen due to its global burden (6.93 million DALYs in 2020), transmissibility via aerosols, diagnostic gaps, and the complexity of treatment.
- MRSA remains a high priority.
- There is a notable increase in recognition of “community” pathogens like fluoroquinolone-resistant Salmonella Typhi, non-typhoidal Salmonella, and Shigella spp., which have moved up in priority due to increasing resistance and substantial burden, especially in LMIC.
- Fluoroquinolone-resistant Salmonella Typhi is now high priority, with an estimated 10 million cases and 116,800 deaths annually.
- Increased resistance to fluoroquinolones in non-typhoidal Salmonella is a major global concern and can indirectly increase resistance in Salmonella Typhi.
- Fluoroquinolone-resistant Shigella spp. moved from medium to high priority due to the high burden of diarrheal mortality.
- MDR N. gonorrhoeae remains high priority due to its high burden, transmissibility, and increasing resistance to recommended treatments.
–Implementation and Policy Considerations:
- The WHO BPPL is a global tool, but there are significant regional and local differences in pathogen distribution, ecology, and AMR. Regional and local contexts must be considered for effective action.
- A syndromic (disease-focused) approach to R&D could be beneficial for high-burden community pathogens like Salmonella, Shigella, and N. gonorrhoeae, targeting the clinical diseases they cause rather than just individual resistant strains.
–Rifampicin-Resistant Tuberculosis (RR-TB) Specifics:
- RR-TB is a major cause of ill health and death, and a leading cause of death due to AMR.
- The non-fatal health burden of RR-TB was substantial, accounting for 6.93 million DALYs in 2020, with significant long-term morbidity for survivors.
- M. tuberculosis is transmitted through exhaled aerosols, and the transmissibility of DR-TB is not significantly different from drug-susceptible TB. Most RR-TB cases result from primary transmission.
- In 2021, there were an estimated 450,000 incident cases of MDR/RR-TB globally, with considerable regional variation.
- Preventing RR-TB involves preventing acquired resistance through effective therapy, reducing primary transmission via infection control, and minimizing progression from infection to disease.
- Significant gaps remain in RR-TB diagnosis and treatment coverage.
- The clinical development pipeline for new anti-TB drugs and regimens is active, with several candidates in various phases of trials.
Conclusion
The WHO Bacterial Priority Pathogens List provides a crucial framework for prioritizing global efforts to combat antimicrobial resistance. The continued critical priority of Gram-negative bacteria and the significant inclusion of RR-TB highlight the urgent need for research, development, and effective public health interventions targeting these threats. The increased recognition of community pathogens underscores the broadening scope of the AMR crisis. Effective implementation of this list requires consideration of regional and local contexts and innovative approaches to R&D, such as a disease-focused strategy for certain high-burden pathogens. Addressing the challenges posed by these priority pathogens is essential to safeguard public health and ensure the continued efficacy of modern medicine.
Credit for image: WHO
Citation: WHO Bacterial Priority Pathogens List, 2024: bacterial pathogens of public health importance to guide research, development and strategies to prevent and control antimicrobial resistance. Geneva: World Health Organization; 2024. Licence: CC BY-NC-SA 3.0 IGO.