Disclaimer: This post is for academic purposes only. Please read the original document if you intend to use them for clinical purposes.
This document summarizes the key information and main themes presented in the Communicale Disease (CD) alert regarding Scrub typhus published in August 2024 by National Centre for Disease Control (NCDC) of Director General of Health Services (DGHS), Government of India. The document provides an overview of the disease, its epidemiology in India and globally, clinical presentation, diagnosis, treatment, and prevention and control strategies. The information is crucial for healthcare professionals and public health administrators to effectively manage and mitigate the impact of this re-emerging infectious disease.
Main Themes and Important Ideas/Facts:
- An emerging and re-emerging Threat:
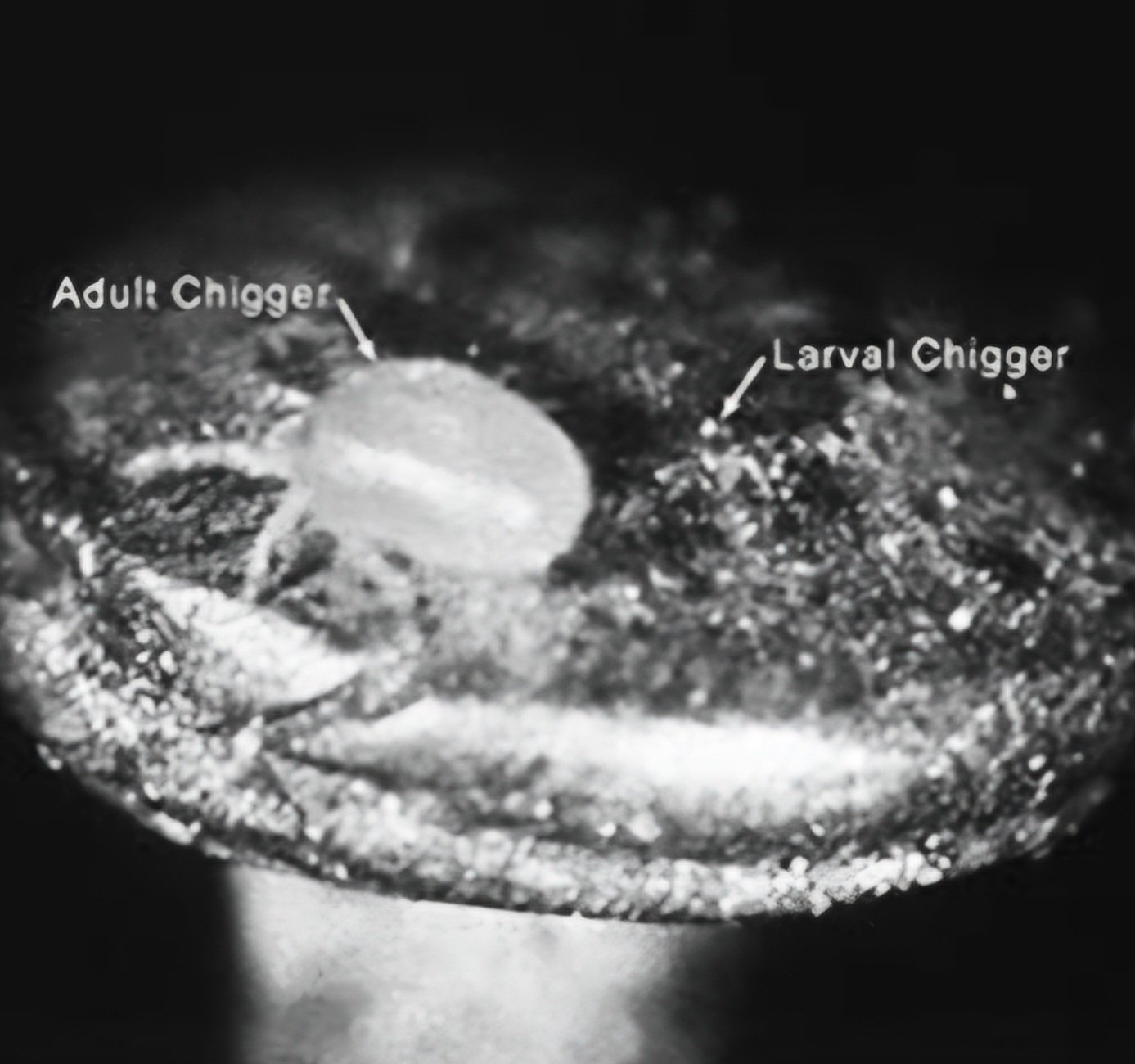
- Scrub typhus is identified as an acute, febrile, infectious illness caused by Orientia tsutsugamushi, transmitted by the bite of infected Leptotrombidium mite larvae (chiggers). It is a zoonotic disease where humans are accidental hosts.
- The NCDC highlights that Rickettsial diseases are considered some of the most covert emerging and re-emerging diseases and are being increasingly recognized in India.
- Scrub typhus is now recognized as the commonest occurring Rickettsial infection in India.
2. Global and Indian Epidemiology:
- Globally, Scrub typhus is endemic to the “tsutsugamushi triangle” in the Asia-Pacific region, with an estimated one million new infections annually and over one billion people at risk. The vector is present in most South-East Asian countries, including India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, and Thailand.
- In India, Rickettsial diseases have been documented since the 1930s. Recent increased awareness, better diagnostics, and improved surveillance have led to wider detection across various states, including the north-eastern states, Jammu and Kashmir, and many others in the north, east, west, and south.
- NCDC notes that in some regions, Scrub typhus accounts for up to 50 per cent of undifferentiated fever presenting to hospital.
3. Changing nature of outbreaks in India:
- Outbreaks are no longer confined to specific terrains or small foci.
- Large numbers of susceptible individuals can be infected simultaneously over short periods.
- A history of arthropod bites may not always be easily recalled by patients.
- A key characteristic is the rapid response to treatment to Tetracyclines/ Macrolide group of drugs.
4. Transmission dynamics:
- Orientia tsutsugamushi is a gram-negative bacterium with significant antigenic variation among serotypes.
- Transmission occurs through the bite of infected chiggers mites found in specific soil microecosystems (mite islands). Only the larval stage feeds on the serum of warm-blooded animals, including rodents, which act as natural reservoirs.
- The bacteria are transmitted transovarially in mites, maintaining the infection cycle.
- Leptotrombidium deliense group of mites is widely distributed in India, coexisting with rodents.
- Risk of encountering infected chiggers is higher in rural populations involved in farming but is increasingly reported in urban areas with exposure to rodents or during outdoor activities.
- Disease seasonality in India correlates with mite activity.
5. Clinical presentation:
- The incubation period is 5-20 days (average 10-12 days).
- The chigger bite is often painless, and an eschar is often seen in humans at the site of the chigger bite typically in concealed areas. However eschars are rare in patients in countries of South-East Asia.
- The illness onset is sudden, with symptoms like shaking chills, fever, severe headache, conjunctival infection, and lymph node swelling. A spotted rash on the trunk may be present.
- Complications of more virulent strains can include haemorrhage, intravascular coagulation, atypical pneumonia, ARDS, encephalopathy, myocarditis, DIC, and MODS.
- Case fatality rate of scrub typhus can be as high as 30-70% if no appropriate treatment is received.
6. Case Definition and Differential Diagnosis:
- Suspected/clinical case: is defined as an acute undifferentiated febrile illness of five days or more, with or without eschar. Fever of less than five days with eschar should also be considered.
- Differential diagnosis includes Dengue, Malaria, Pneumonia, Leptospirosis, and Typhoid.
- Probable case: involves a suspected case with significant titres in Weil-Felix test or positive IgM ELISA.
- Confirmed case: requires a clinical description compatible with scrub typhus and either high IgM antibodies in ELISA, a four-fold rise in Weil-Felix titres, or seroconversion on ELISA/IFAT.
7. Laboratory Diagnosis:
Diagnosis relies on serology (Weil-Felix, ELISA, IIF), molecular diagnosis (PCR), and, less commonly, organism isolation. Serological assays are the simplest & mainstay diagnostic tests for rickettsial diseases.
- The Weil-Felix test is commonly used and has reasonable sensitivity and specificity as per NCDC experience.
- ELISA, particularly IgM and IgG capture assays, are considered probably the most sensitive tests available. IgM indicates recent infection.
- PCR on clinical specimens can be used for direct detection of O. tsutsugamushi DNA, especially in the first week of illness.
- Organism isolation is not for routine diagnosis due to its infectious nature and requires specialized biosafety level 3 laboratories.
8. Treatment:
Prompt institution of effective antibiotic therapy against rickettsiae is the single most effective measure for preventing morbidity and mortality.
- Tetracyclines (e.g Doxycycline) and Chloramphenicol are proven therapies. Macrolides (e.g. Azithromycin) are an effective alternative.
- Treatment should be initiated based on clinical suspicion, without waiting for lab confirmation. Specific dosage recommendations are provided for adults, children, and pregnant women (Azithromycin is the drug of choice in pregnancy).
- In complicated cases, intravenous doxycycline, azithromycin, or chloramphenicol may be used.
- NCDC notes that Doxycycline and/or Chloramphenicol resistant strains have been seen in South-East Asia. These strains are sensitive to Azithromycin.
- Caution is advised regarding Tetracycline use in children under 8 and pregnant women due to potential side effects.
- Chemoprophylaxis: Pre-exposure chemoprophylaxis with Chloramphenicol or Tetracycline (for short periods of high-risk exposure) or weekly Doxycycline (in children) is recommended.
9. Prevention and Control Strategies:
No effective human vaccine is currently available due to the organism’s serotypic heterogeneity. Preventive measures for the general public include wearing protective clothing, using miticides on clothing and bedding, applying insect repellents (DMP, Benzyl benzoate, DEET), avoiding sitting or lying on bare ground, and using ground covers. Environmental control measures include vegetation clearing and chemical treatment of vegetation/soil.
Control strategies emphasize:
- Rapid case identification by Health-care workers (HCWs) can help provide prompt treatment. This includes prepositioning diagnostic kits.
- Public education on case recognition and personal protection.
- Rodent control through various methods (trapping, poisoning, natural predators) and “Habitat modification such as good sanitation.
- Vector control via insecticide treatment.
Conclusion:
The CD alert by NCDC highlights the significant public health threat posed by Scrub typhus in India. The document emphasizes the increasing recognition and widespread distribution of the disease, the potential for severe outcomes if untreated, and the importance of early clinical suspicion, accurate diagnosis, and prompt treatment with appropriate antibiotics. The alert also underscores the need for public health interventions focusing on prevention, control of vectors and reservoirs, and public awareness to mitigate the burden of Scrub typhus in the country. The information provided is critical for guiding healthcare practices and public health strategies at various levels.
Credit for image: CDC