Disclaimer: This post is for academic purposes only. Please read the original document if you intend to use them for clinical purposes.
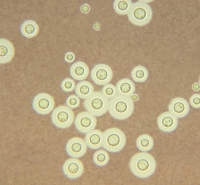
🦠 Cryptococcosis Treatment Algorithm
Global Guidelines for Diagnosis and Management | Evidence-Based Recommendations
🧠 CNS Cryptococcosis
🔄 Disseminated Disease
(Non-CNS/Non-pulmonary)
🫁 Pulmonary Disease
With/Without Cryptococcoma
🩹 Direct Skin Inoculation
Cutaneous infection
💊 PRIMARY INDUCTION THERAPY
🎯 INDUCTION PHASE
🔄 CONSOLIDATION PHASE
Fluconazole 400-800 mg daily
Duration: 8 weeks
(800 mg preferred in low-income settings)
🛡️ MAINTENANCE PHASE
Fluconazole 200 mg daily
Duration: 12 months
(Until immune restoration)
📋 Treatment Durations by Disease Type
⚠️ CRITICAL MANAGEMENT POINTS
• Delay ART initiation 4-6 weeks
• Monitor for C-IRIS
• Screen with CrAg if CD4 <200
• Therapeutic lumbar punctures for ↑ICP
• Therapeutic drug monitoring for calcineurin inhibitors
• Carefully adjust immunosuppression
• Monitor for drug-drug interactions
• Extended treatment duration
• Therapeutic lumbar punctures if pressure ≥20 cm CSF
• Remove CSF to reduce pressure by 50%
• Surgical drainage if refractory
• Avoid acetazolamide, mannitol
• CBC, renal function, electrolytes q48h
• Pre-hydration with amphotericin B
• Aggressive K+ and Mg2+ replacement
• Flucytosine levels if available
• Amphotericin B formulations are safe
• Avoid flucytosine (Category C)
• Avoid fluconazole (Category D)
• Especially avoid in first trimester
• AmB 1 mg/kg or liposomal AmB 3-4 mg/kg
• Flucytosine 100-150 mg/kg/day in 4 doses
• Fluconazole 12 mg/kg daily (max 800 mg)
• Weight-based calculations essential
Key Clinical Pearls
- Early Recognition: Consider cryptococcosis in any immunocompromised patient with compatible symptoms, regardless of HIV status
- Lumbar Puncture is Essential: All patients with suspected cryptococcosis require LP with opening pressure measurement
- Combination Therapy Superior: Amphotericin B + flucytosine combination shows superior early fungicidal activity compared to monotherapy
- Pressure Management Critical: Raised intracranial pressure is a major cause of morbidity and mortality – aggressive management with therapeutic LPs is essential
- ART Timing Matters: In HIV patients, delaying ART initiation by 4-6 weeks reduces C-IRIS risk and improves outcomes
Clinical Decision Making
This algorithm represents a synthesis of evidence from multiple randomized controlled trials and expert consensus from over 70 international medical societies. Treatment decisions should always be individualized based on:
- Patient immune status and comorbidities
- Disease severity and extent
- Local antifungal availability and resources
- Potential drug interactions and contraindications
- Monitoring capabilities
When to Consult Specialists
- Infectious Disease: All cases of cryptococcosis
- Neurosurgery: Refractory increased intracranial pressure
- Ophthalmology: Visual changes or suspected ocular involvement
- Clinical Immunology: Cryptococcosis in apparently immunocompetent patients
Remember: Cryptococcosis remains a medical emergency with high mortality. Early recognition, prompt initiation of appropriate antifungal therapy, and aggressive management of complications are crucial for optimal outcomes.
Citation: Chang CC, Harrison TS, Bicanic TA, Chayakulkeeree M, Sorrell TC, Warris A, et al. Global guideline for the diagnosis and management of cryptococcosis: an initiative of the ECMM and ISHAM in cooperation with the ASM. Lancet Infect Dis. 2024 Aug;24(8):e495-e512. doi: 10.1016/S1473-3099(23)00731-4. Epub 2024 Feb 9. Erratum in: Lancet Infect Dis. 2024 Aug;24(8):e485. doi: 10.1016/S1473-3099(24)00426-2. PMID: 38346436; PMCID: PMC11526416.